There is a lot of information to take into consideration when determining which practices to follow when returning to a physical workplace during the pandemic. The biggest source of confusion is how public health directives/guidelines compare to workplace safety practices, particularly with the use of masks. In our view, public health advice informs workplace health and safety practices but does not overrule the Employer’s legal workplace health and safety obligations, which include taking every reasonable precaution to keep workers safe.
- This document is also available in PDF printable format.
Face coverings are cloth masks that are recommended by public health agencies to prevent the spread of COVID-19. They may be homemade, purchased, donated or sold. They can also be non-medical masks (which would be indicated on the packaging when purchased). CUPE supports this practice and encourages everyone who can tolerate it to wear a facial covering when they are in a public setting, which includes their workplaces (unless greater protections are required by their job).
Medical masks, face shields and respirators are medical devices that are constructed to manufacturing and performance standards and are worn by workers in different circumstances and combinations to protect them while they are working.
Public Health Advice
The healthcare system accepts the fact that, once an illness has been contracted or developed, some patients will die. In this framework, public health agencies focus on the health of the general public and on keeping track of different types of illnesses. They set expectations and recommend practices for general public safety within the framework of acceptable risks. The Public Health Agency of Canada, and provincial and local public health agencies will set out, in general terms, reasonable precautions for members of the public in “low risk” non-workplace settings, or what an individual should do if exposed to an illness or infected by a disease.
Among their other roles, they establish case definitions, the types of precautions required based on the type of risk, establish terms of quarantine and isolation, and establish testing and tracking protocols of reportable communicable illnesses. These undertakings may result in emergency orders being issued by the government. Public Health agencies have no mandate to protect workers while they are working. Therefore, they do not overrule the Employer’s legal occupational health and safety obligations to protect the health and safety of its workers.
Is a face shield as good as mask?
Face shields do not offer the same protections as masks. A mask worn properly protects the worker and other people to varying extents depending on the type of mask. A face shield (medical or otherwise) offers limited protection to the wearer. A face shield does NOT prevent an asymptomatic carrier or a mildly afflicted person from potentially spreading the virus all over the workplace. It does not prevent a virus from getting to the individual that isn’t covered by the shield, and it’s usefulness is dependent on it being worn properly (and often is not). Some shields are disposable, while others are intended to be reused after cleaning and/or decontamination.
Public Health Guidance
Public health agencies across Canada have given the following advice to members of the public to stop the spread of COVID-19:
- Isolate or quarantine if you have symptoms or may have been exposed to COVID-19;
- Wash your hands often (with soap and water for twenty seconds or use hand sanitizer);
- Stay 2 metres (six feet) apart from others;
- Wear a face covering when you’re outside your home (sometimes called universal masking);
- Keep your social circle small.
This advice is suitable for the general public in a setting where there is minimal contact, where people can generally maintain physical distance and with the general public.
Employers have a legal obligation to protect workers
There are different health and safety standards for workers than those for the general public. These must be applied because the risk of transmission is greater when they are in a physical workplace with a greater number of contacts with a greater number of people. Greater worker protections must be implemented when the following conditions may be present where workers are working in:
- Close contact with others (within 2 metres for 15 minutes or more)
- Continuous exposure to others
- Crowds
- Closed or poorly ventilated spaces
- Coverings (where face coverings are not being worn, or not being worn properly)
- Colder temperatures
Employers have a greater responsibility than that of public health agencies when it comes to ensuring the health and safety of their workers. Contrary to the public health strategies which are based on “acceptable risk”, employers have a legal obligation to take all reasonable precautions for the protection of the health and safety of each of their workers. Employers must focus on preventing infection and preventing exposure to the virus. Those obligations are set out in the various health and safety laws across Canada. Public health agencies do not write workplace health and safety policies and programs nor do they perform occupational risk assessments.
Different levels of public health agencies or officials have stated that they cannot or will not mandate that people wear face coverings or masks when outside their homes. However, employers CAN mandate face coverings and masks in their workplaces because they have an obligation to take all reasonable precautions in the circumstances for the protection of workers. That means that they have to take all reasonable precautions to prevent the infection from happening.
In the case of COVID-19, the employer must have safety protocols which are not optional. If workers cannot adhere to certain protocols for medical reasons, then the Employer has an obligation to accommodate them away from the risks to their health and safety. Some employers may accept a worker’s statement and implement work-from-home or alternative work schedules or tasks. Other employers may require documentation from a healthcare provider.
How do public health and occupational safety measures work together?
The public health advice about the universal use of face coverings is comparable to an administrative policy on occupational hygiene. In some jurisdictions or in certain groups, this could be made mandatory by governments through different orders. Some examples include the provincial requirements to mask in schools or healthcare, or when a municipality requires the use of face coverings while indoors or in groups.
These hygiene practices are designed to limit the number of droplets that accumulate in the air that could be inhaled by a worker and make them unwell. Most workplaces have policies and programs with respect to occupational hygiene and may include topics such as scent-free workspaces, ventilation, and hand and cough hygiene. A public health order requiring the universal use of face coverings has the same effect as a workplace policy.
If a worker requires specific protection from a hazard (like directly working with sick patients), then personal protective equipment (PPE) must be provided. PPE is different than other facial coverings because they have been manufactured to a tested standard and must meet performance metrics. PPE requires policies and programs, training and education for workers and provides specific benefits. Remember:
- Face coverings reduce the amount of exhaled breath that accumulate in the work environment.
- Masks do what face covering do, but are designed to protect a worker from splashes and droplets.
- Respirators protect against inhaling contaminants in the air, and some models can protect against splashes.
How everyone wearing a face covering helps
Universal masking in a workplace is a hygienic method designed to prevent a person from accidentally contaminating the environment from mouth or nasal excretions, like when breathing, talking, coughing or sneezing. It’s the equivalent of coughing into an elbow or tissue, except it’s much more convenient and effective. Using this administrative hygiene policy, a workplace may also prevent spread of communicable illnesses from pre-symptomatic and asymptomatic individuals. This policy should be applicable to everyone coming into the workplace to be effective. If not, then all the surfaces surrounding an unmasked person should be disinfected. Scientific evidence demonstrates quite clearly that a cough or sneeze can travel much farther than 2 metres (six feet).
The following figures illustrate how face coverings could be used to prevent COVID-19 spread in the environment.
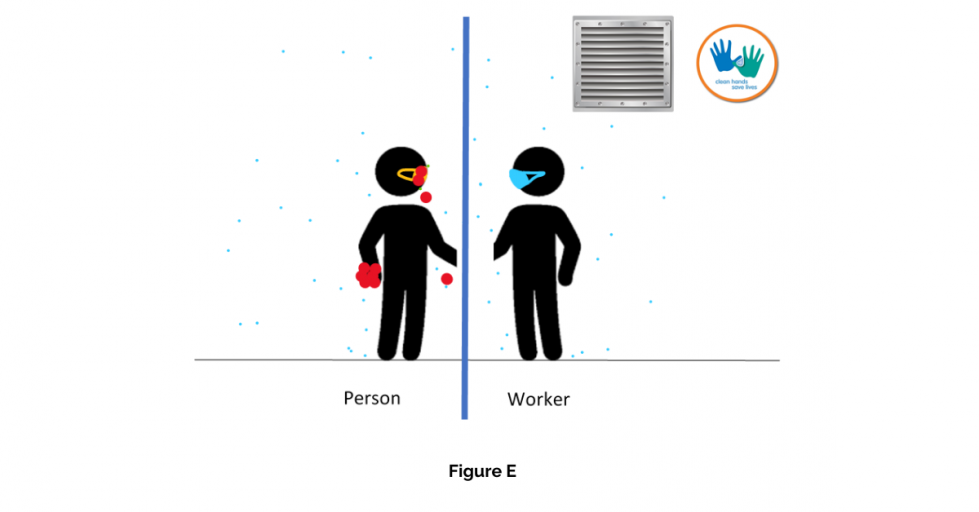
Figure A – a worker is meeting with a person, nothing said yet
There are always particles floating in the air, whether we can see them or not (blue dots). Depending on the size and weight of those particles, they will either stay floating in the air, or they will slowly make their way to the floor. (Things that are on the floor (or other surfaces) can be resuspended in the air, but it’s not likely to be a significant source of infection of COVID-19.)
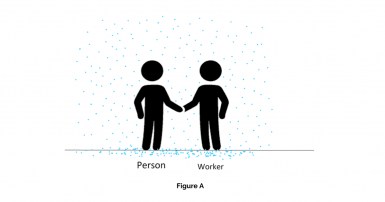
Figure B –A conversation starts
When a person is speaking, there are things that come out of their mouth (green dots). Air currents in the space where this happens will affect where those things end up. In most office settings or places where you wouldn’t expect wind and the air is fairly still, particles in exhaled breath will make it to the worker’s airways. If you can smell someone’s breath, you are inhaling things from their mouth. Some of those particles coming out of a person’s airways will drop to the ground, while others can stay suspended in the air.
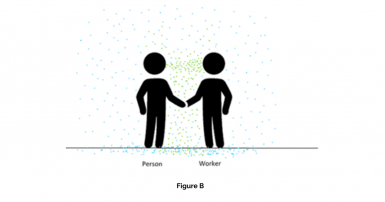
Figure C – A person is infected with COVID-19
It is possible that a worker working with the public will come into contact with a person who is infected and either pre-symptomatic or asymptomatic. Virus particles can come out from a person while they are speaking, breathing, singing, coughing and sneezing, for example (red dots). They will either join other particles on the floor or surfaces (where they could be resuspended if not cleaned often enough) or stay suspended in the air.
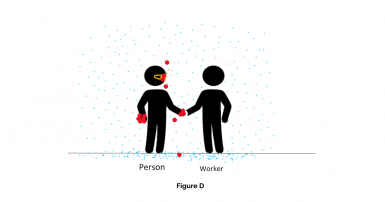
Figure D – Masking as a hygiene principle
A face covering (yellow) on the person who is infected but may not know it, can reduce the risk to the worker significantly because it is catching most of the droplets (and hopefully the virus) on the face covering. Face coverings are not perfect, but they help.
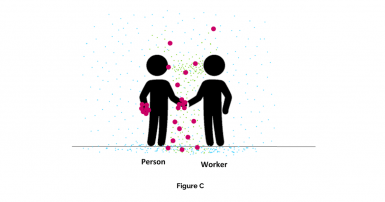
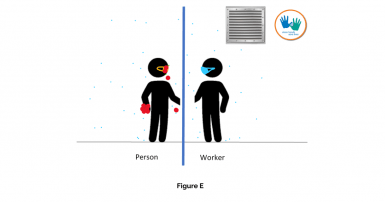
Figure E – Layers of workplace protections
Adding more layers of protections will reduce the risk of transmission even more. Some of those interventions may include PPE for the worker (like a surgical/procedural mask in blue), frequent hand hygiene, increased ventilation, increased disinfecting of surfaces and preventing direct contact by physical distance or barriers (blue barrier between worker and the person they are providing service to).
Definitions
Asymptomatic: a person is infected but does not have any noticeable symptoms. This person is impossible to find without a COVID-19 test but can infect other people if prevention measures are not taken.
Pre-symptomatic: a person who is infected but has not yet developed symptoms. A person infected with COVID-19 can spread the virus and infect other people up to 2 days before they develop symptoms.
Incubation period: the period of time after exposure to the virus but before symptoms show up. Fifty percent (50%) of infected people will show COVID-19 symptoms as of Day 5 after the exposure event. Ninety-five percent (95%) of infected people will have developed symptoms by Day 14 after the exposure event.
Hand Hygiene: the practices that a person takes to keep their hands healthy and free of virus. This could be washing hands with soap and water, using an ethanol-based hand sanitizer, avoiding touching surfaces that could be contaminated, not touching your face or your mask etc.